22 Oct Breast Cancer Reconstruction Awareness, Choices, What to Know
Little did I know I would become so well-versed in the various breast reconstruction options.
It seemed straighforward, if not overwhelming, at the start: breast cancer diagnosis, immediate double mastectomy with expander placement, followed by exchange to implants 2 months later.
But things didn't go as planned, and I was definitely not prepared for the long and painful road I would have to take to get to where I wanted to be with breast reconstruction.
Today is Breast Reconstruction Awareness (BRA) Day
Most of you, like me, have probably never heard of "Breast Reconstruction Awareness" (BRA) Day until now.
BRA Day began as an awareness campaign by the American Academy of Plastic Surgeons and The Plastic Surgery Foundation with a purpose to:
"Educate, engage and empower women to make the decision that is best for them following a diagnosis of breast cancer," which "involves informing women, family members, caregivers and the media that the breast cancer loop remains open until a woman is informed of breast reconstruction options." (PSF Website, 10/20)
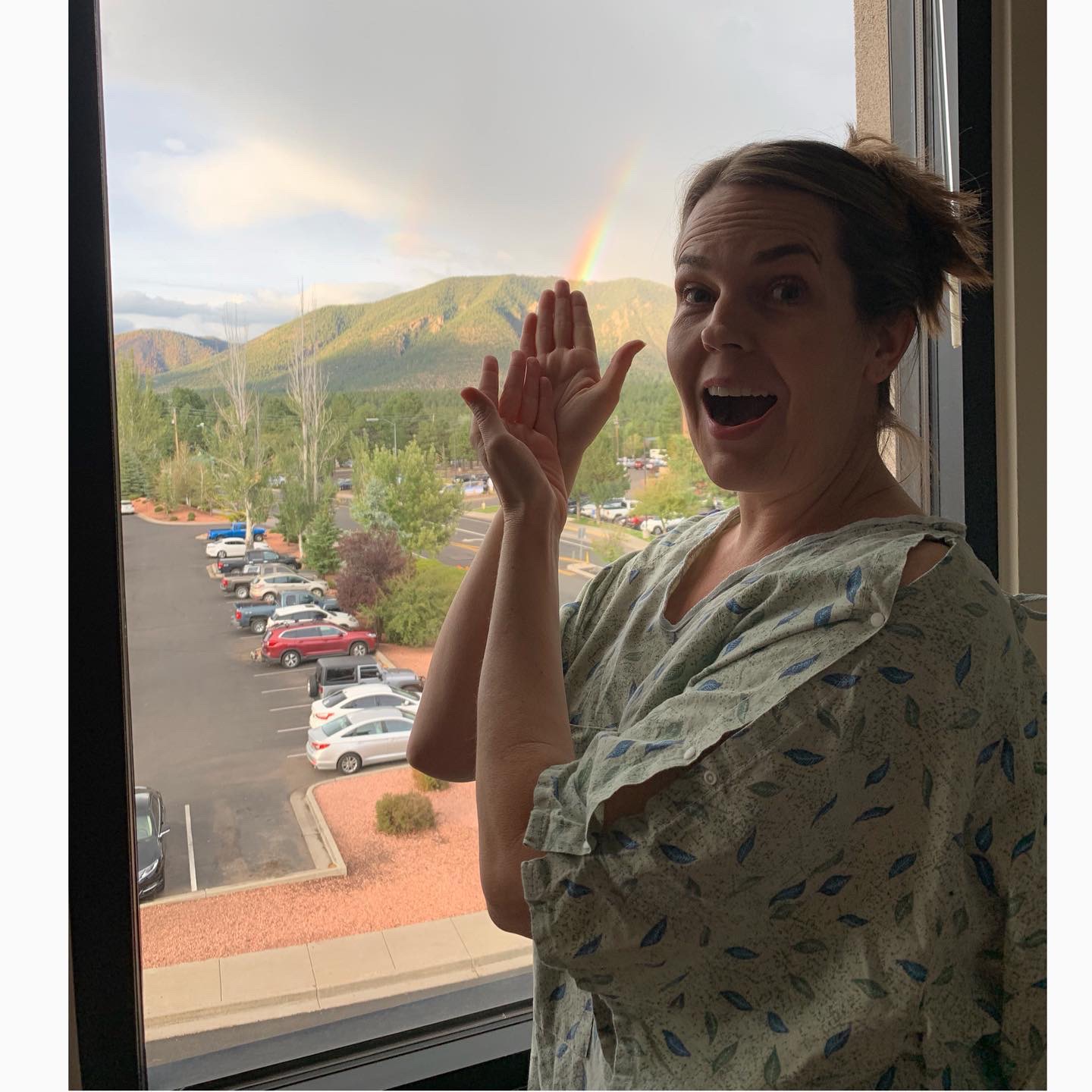
In the hospital with my first implant infection, trying to see the "good" and focus on the rainbow and not the rain.
"The breast cancer loop remains open..."
Wow, does that resonate with me!
When we don't have all the options for breast reconstruction, when we don't have all the information, we can go in circles.
That's exactly how I've felt these past 15 months--like I have first been de-constructed over and over, stripped down to nothing, dismantled part by part (not only from surgeries; chemo is really good at dismantling you, too!).
Then, I've had to start reconstruction over and over--again and again, in a constant loop--surgery by surgery, infection by infection, decision by decision.
It's such a personal decision...
To reconstruct or not following a double mastectomy is a monumental and extremely personal choice each mastectomy patient must make.
The trouble is, most of we breast cancer warriors are so overwhelmed by our diganosis, prognosis, and treatment plan (which is often immediate and all-consuming), we simply don't know what we don't yet know.
We don't know the right questions, the different types of procedures, our complete list of options.
Well-meaning surgeons and oncologists lay out their "best option" treatment plans, and most of us go along with it, because we trust our surgeons and oncologists, and because "this is what's done," as far as we know.
We don't know any other way yet; it's all new and overwhelming.

The morning of my double mastectomy, watching the sunrise, trying to figure out what was happening to me, in only 7 days from diagnosis.
That's how I felt when I began my reconstruction journey....
With my double mastectomy exactly one week following my stage 1, invasive ductal carcinoma, triple negative, breast cancer diagnosis, I had no time to process, understand, or really come to grips with anything.
I just knew I was likely BRCA1 positive (later confirmed by genetic testing), which meant I carried the BRCA gene mutation, putting me at high risk of a breast cancer recurrence or metastasis and several other cancers, too. Since triple negative is the most aggressive and deadly type of breast cancer, all I knew was I needed it out of me before it spread.
I was beyond grateful to my breast surgeon for getting me in so swiftly and giving me my life, essentially. Dr. Beth Dupree is a pioneer of the "nipple-sparing mastectomy," and I was blessed to have this option successfully carried out by someone so skilled. I knew I was in excellent hands.
I also felt completely surreal through the entire process--like I was watching a movie of someone going through these experiences.
My mind and body were in survival mode, and I was numb to it all. I simply couldn't process what it meant to have my breasts AMPUTATED--because that's what it IS--an amputation.
I had even less preparation to comprehend the breast reconstruction process....
With immediate placement of expanders during the double mastectomy surgery, I just did what I was told, again, because it seemed to be "what was done," it seemed to be THE way.
And it was for me...for a while.
My breast reconstruction story is anything but short, or "THE way."

Immediately following my double mastectomy with expander placement. So sore. So out of it. My chest feeling empty and like rocks are filling it at the same time.
*July 24, 2019--Double mastectomy with expander placement
*2 Weeks later--Begin expander "fills" (to stretch the skin gently in preparation for the desired size of implants)
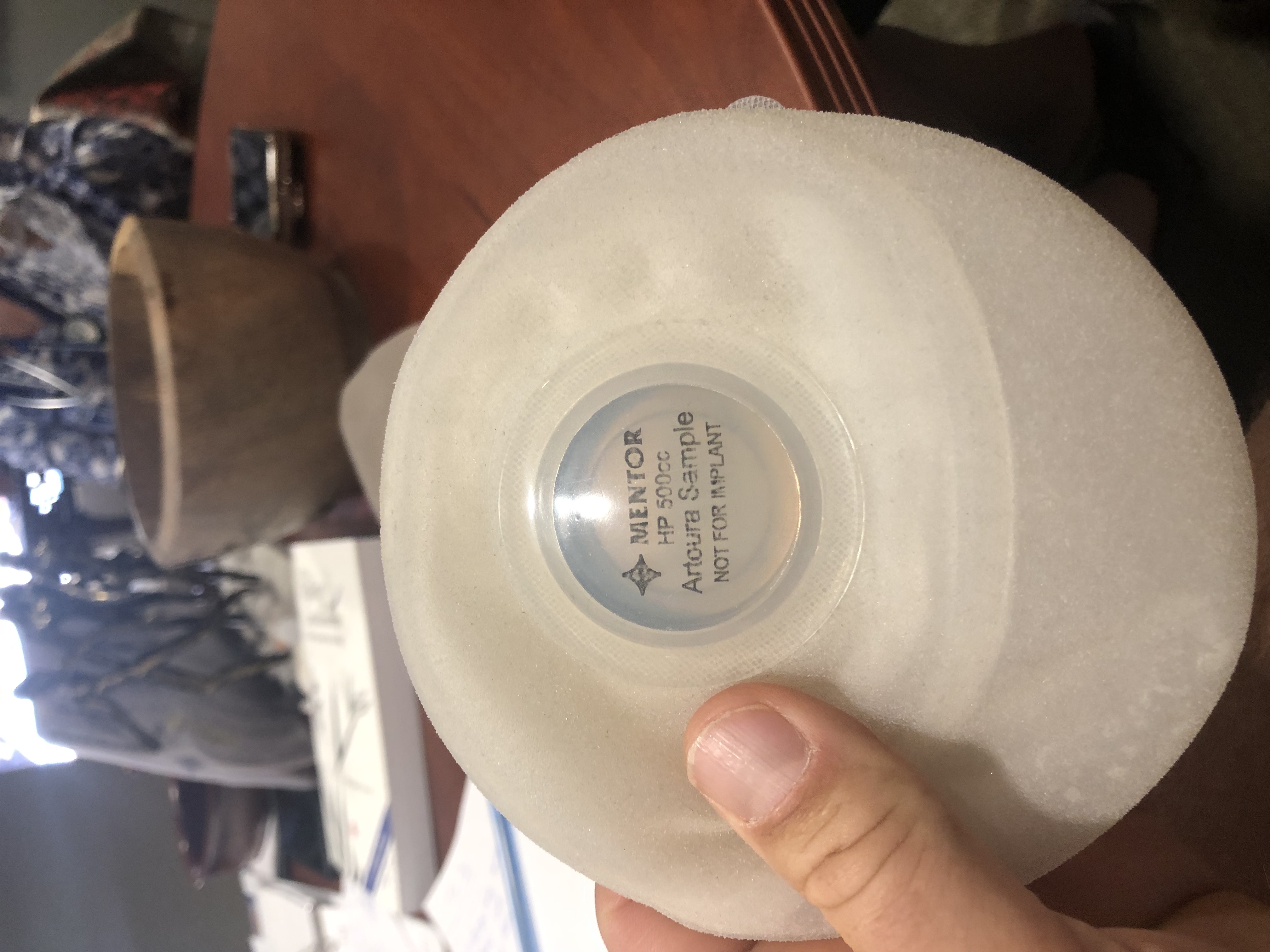
This is an unfilled expander. Hard plastic, with a metal "port" the plastic surgeon inserts a needle into and "fills".
*Sept 12, 2019--Exchange filled expanders for implants (AND full hysterectomy. Due to my BRCA1 status, I'm at high risk of ovarian, fallopian tube, and other cancers. I thought I'd do my "2 surgeries at once," to be "done" with surgery. Little did I know...!)

After my implant exchange, thinking I was "done" with surgery, just about to get my first infection.
*10 Days Later--Developed a staph infection in my right breast. 6 days in the hospital trying to fight it with IV antibiotics, & finally....
*Sept 28, 2019--Right implant removed
*Oct 10, 2019--Began chemotherapy and cold-capping to save my hair.
*December 5, 2019--Left implant removed, due to infection in left breast from weakened system from chemo

The night before my left "explant" surgery, after living with one breast for 3 months I was about to lose the other.
*December 16, 2019--Last chemo
*January 2020--Developed blood clots from chemo, started blood thinners that made me bleed
*February 2020--Discovered bleeding was from large kidney stones (from chemo, too)
*March 2020--Lithotripsy surgery to blast kidney stones
*May 5, 2020--Expander placement surgery, attempt 2.
Ready to try expanders one more time (because it seemed like a "fluke" I picked up a staph infection and the other infection was due to chemo). Surgeon said I had an extremely low likelihood of developing a 3rd infection and it was incredibly rare to even have had 2!
10 days later--Staph infection in left breast.
May 15, 2020--Emergency surgery to exchange infected expander for a new one and "clean" infected area. Antibiotic beads placed inside breast.
6 weeks following--Intense antibiotics that eventually "cured" the staph infection. Both my surgeon and I knew it was a miracle it had actually worked.
*June 29, 2020--Exchange surgery from expanders to implants, round 2. All seems to be going well--my "easiest" reconstruction surgery so far.
*10 days later--Start seeing signs of infection in left breast again, and immediately start antibiotics.
At this point I know if we can't "save" the implant, I'm "done" with trying implants. My plastic surgeon says, "Some women's bodies just don't like foreign devices."
I know that if the implants fail, I'll either need to stay flat OR do "an intense flap surgery that's a much bigger deal," as I understood it. I was scared of that option, and praying implants would work. (My plastic surgeon is also stumped as to why I have been so unfortunate and had so many staph and other infections. He says he's never heard of this happeneing to anyone in all his years.)
*And...the infection gets better.
So, I keep the implants and start healing and hoping I am FINALLY going to start moving on from this year-long (at this point) ordeal.

When I started wondering about Breast Implant Illness, after my 7th surgery, with skin sores and rashes and body and joint aches, so very exhausted.
*Enter Breast Implant Illness...
There is much to say about Breast Implant Illness (BII), and I will do so in a separate article.
Bottom line for me is: I developed symptoms I first thought were infection-related (skin redness and rashes, a fungus on my leg, headaches and pain in my breast area), and other symptoms that were new to me--headaches, blurry vision, and joint pain that started in my ankles, and progressively worsened in my knees, hips, and elbows.
The implants were making me sick.
I felt the truth of this weeks before I or anyone around me was convinced of it, and I knew what it meant: 1) THIS explained why I was getting infection after infection around my expanders/implants, and 2) I'd need to have my implants removed. More surgery.
And did I want to try the "flap" reconstruction, with all its scary consequences and complications? Or did I just want to stay "flat and fabulous" as many women choose to do?
I had been "flat" for 5 months, after being "one-breasted" for 3 months, and honestly, I felt anything but fabulous. Especially with the nipple-sparing mastectomy--my skin and nipples sort of curled up in a lumpy awkward chest I did NOT feel comfortable in.
*Enter DIEP Flap Reconstruction
I finally decided to do the DIEP Flap Reconstruction, with a plastic surgeon I could trust who's done over 1000 with a less than 1% failure rate. (Dr. Raman Mahabir, Scottsdale, AZ)
This surgery involves opening the abdomen, hip to hip, and removing tummy fat and skin, opening the breasts (again) and placing the fat inside the breast pocket, taking an artery from the tummy and reattaching it inside the breast (microsurgery), and sewing everything back up.
*My DIEP Reconstruction was Sept 18, 2020. It was my 10th surgery.
Yes, I had complications.
A drain leaking blood all over required surgery again the day after my 9 hour DIEP surgery, to replace the drain.
* And one week after my DIEP, I ended up in the ER, then an ambulance driving me 2 hours from Flagstaff to Scottsdale AZ where I had emergency abdominal hernia surgery.

In the ER exactly one week after my 9 hour DIEP Flap surgery, told I had a hernia and my "intestines were everywhere". Emergency abdominal surgery (again) the next day.
I was in the hospital twice for 5 days at a time.
*My total surgery count in 15 months now is 12.
I've been "home recovering" for 3 weeks.
And yes, I got another staph infection--this time in my hip drain site, and thank goodness it has responded to antibiotics.
So far....
The Bottom Line on Breast Reconstruction...
1) Choosing to reconstruct or not after a mastectomy should always be an option.
And it's a choice to be made ONLY by the woman primarily, and her loved ones and medical team. She should ALWAYS be offered a CHOICE.
2) ALL reconstruction options should be laid out for the patient from the beginning.
Some may choose to go straight for a flap reconstruction, because they don't want implants in them.
Others will decide on expanders to implants.
Whatever each woman decides, she should have the CHOICE to decide between ALL viable options. AND, she should be supported by her doctors whatever her choice.
3) Sometimes, you only know what's really right for you by going through all the complications.
I was told about breast implant illness at the start of my journey. I asked my plastic surgeon about it, and he explained it only happens rarely. I thought my body was "healthy and strong"; little did I know how sensitive my body truly is.
Had I not gone through the expanders and implants and failures and infections, I would never have gotten to where I am now with the DIEP flap. I truly believe it's the RIGHT choice for me, long term.
4) Each breast reconstruction journey is unique.
A mastectomy is ROUGH in and of itself. It requires a lot of tender care, self-compassion, and patience to fully heal. Whether a woman chooses reconstruction or not, it will be a tough journey.
AND no two women have the exact same journey. Even if they choose the same breast reconstruction option, their surgeries, drains, complications (or not), time healing, chemo or radiation routine and how these affect everything will be UNIQUE.
Not everyone will experience all the complications I've had to endure (thank goodness!).
Most will have a smooth breast reconstruction path--choosing the best option, moving forward, and finding they are pleased with their decision, whether it be to reconstruct or not.
Some WILL have complications, and they will get through them with the help and support of family and good doctors.'
A few will have MULTIPLE complications, like me. It will start to feel like "Nothing can ever go right," like you're cursed, like you'll never actually heal and move forward.
No matter YOUR journey of breast reconstruction, believe me when I say: "You do what's BEST for YOU. Be patient. Let your body FULLY HEAL. And DON'T GIVE UP if things get messy. Remember, this is YOUR personal journey. You are the expert of your own body. Fight for what you know is right for YOU. And know YOU'RE NOT ALONE."
(Join my "Growing Through Breast Cancer" Emotional Support FB Group for monthly virtual support meetings, http://www.facebook.com/groups/growingthroughbreastcancer)

So sick from chemotherapy, smiling through the suffering, wishing I could make a difference in the world again.
Finally, Know...
Breast Reconstruction is not an event; it's a process.
I have learned just how long and arduous that process can be for many women.
For ALL women, it's an incredible loss; it's a process of coming to terms with the physical loss, dealing with the emotional loss, and mentally coming to understand what has happened, what we truly WANT with reconstruction, how it will impact our life, and WHO WE ARE with this brand new body.
It's something I'm still figuring out everyday.
Got something to say/ask about breast reconstruction or breast cancer? Leave a comment below!
Join my "Growing Through Breast Cancer Emotional Support FB Group for monthly virtual support meetings, here: http://www.facebook.com/groups/growingthroughbreastcancer










Wow you are a rock star for going through all the complications and coming out stronger and better! I have studied your journey to prepare me for my own. Thank you for being so transparent for people like me to lean on. I’m not there yet, sharing my story with everyone. I hope to have the courage one day so i can also help people like you have.
I’m doing 6 rounds and finished one round. Doing cold caps and i realized the actual cold capping is not the hard part, its the in between rules, wow so many rules. Did you stick to all of them? Looks like you kept all of your hair, even braiding your hair during the process. I am so scared of even touching my hair, i am shedding right now and that is also freaking me out…
anyway, i am so happy to see how successful your outcome was. Give me hope. I know you are having a tough go at it at the moment, just know you are helping so many women out here, sharing your vulnerabilities. Thank you again and hang in there, you are truly a warrior.
Thank you for much for these kind words. I am sorry it took so long to see your comment. I hope you are doing well with all your chemo and capping and everything. It is SO much to go through, but I feel, in the end, it is so worth it. Yes, I was able to keep almost all my hair. Probably lost 20% or so, but it was thick to begin with, so only I can tell the difference. And yes, I agree. Capping isn’t the hardest part. It’s the caution we have to take in between. I did stick to the rules pretty strictly. Keeping my hair braided helped a ton, though I got so sick of it! And I only washed 2ce a week, and very gently. I used the leave in conditioner to help brush out my very tangle-proned hair, and then brushed super gently, holding at the roots, using a WetBrush. SO much fear and worry about everything, and when you add your hair into it, it can be overwhelming. I really hope it is working for you.
Thank you again for your message. I am still not “done” with all of what I now call “Breast Cancer Treatment TREATMENT,” but I am grateful to be alive, to have such a wonderful pink sisterhood community with beautiful people like you. So much love… Christi