07 Aug The Facts vs. The TRUTH about Postpartum Depression (+ video)
The fact is that Postpartum Depression (PPD) is real. I know, because I’ve experienced it four times, along with Postpartum Anxiety. That’s another fact: “Postpartum Depression” is often used as a catchall phrase for a whole spectrum of pregnancy and postpartum mood and anxiety disorders, including OCD, PTSD, and even Psychosis.
PPD: Fact vs. The Truth
As a clinical psychologist and expert on Perinatal Mental Health, I’ve definitely learned about, and seek to share, the facts on Postpartum Depression. I believe everyone should learn about PPD, because chances are either you or someone you know will experience PPD at some point (that’s another fact: as many as 1 in 5 will experience postpartum depression), and knowing the facts can make all the difference. If you want the facts about Postpartum Depression/Anxiety, the following links are a great place to start:
Pregnancy & Postpartum Emotional Health
Postpartum Depression Treatment
Beyond Depression: Understanding Postpartum OCD (part 1, plus video)
Postpartum Depression Treatment: For Dads & Partners
However, as a mother of six who’s experienced Postpartum Depression/Anxiety four times, and as one who has worked with pregnant and postpartum women for over 16 years, I know that sometimes, the facts don’t reflect the full truth about PPD.
20 Truths about Postpartum Depression (plus bonus video!)
The truth is Postpartum Depression is a life-altering experience, and if we really want to understand this experience, we must move beyond the facts and start talking about the truth. Here are 20 truths I’ve discovered about PPD. I hope you’ll learn them, share them, and then join the truthful discussion, below.
1) It can feel like you’re all alone, but you’re definitely not. Postpartum Depression and Anxiety often feel isolating; it feels like you’re the only one feeling this way. The truth is you’re not alone. Most women will experience some change in their emotional health following childbirth (up to 80%), and one in five will experience a perinatal mood or anxiety disorder. Because of this, PPD has been called the most common complication associated with childbirth.
2) PPD is not your fault. There are many risk factors that make Postpartum Mood/Anxiety Disorders out of your control, not least of which include: the extreme changes in hormones (women who are sensitive to hormonal shifts are definitely at higher risk), the insanity that is sleep deprivation (women sensitive to sleep loss are at higher risk), and the coping and adjustment that naturally comes when a new baby is born. The list of risk factors is long, and bottom line: Even if you feel like it’s your “fault,” it’s not.
Watch this “3-Minute Therapy” video from my YouTube channel on “The Truth about Postpartum Depression,” then continue reading, below.
[stream provider=youtube flv=http%3A//www.youtube.com/watch%3Fv%3D-i94cc8TCEw img=x:/img.youtube.com/vi/-i94cc8TCEw/0.jpg embed=false share=false width=640 height=360 dock=true controlbar=over bandwidth=high autostart=false responsive=16:9 /]
3) Postpartum Depression is not a character flaw, and it does not mean you are weak. For many women, however, it feels that way. The more we talk about and educate people on PPD, the more women will see PPD for what it is: an illness that comes, and, with help, will go, just like any other. (Read Postpartum Depression Treatment)
4) Postpartum women are far more exhausted than you, or they, realize, and sleep plays a critical role in PPD, and its treatment. You can’t understand how exhausted you can be until after you have a baby. Postpartum depressed or anxious women often also suffer from insomnia; the baby is sleeping through the night, but she is not. Sleep is crucial to mental and emotional well-being, and helping moms treat sleep issues is a crucial part of them becoming well again. (Read: PPD Treatment–Sleep)
5) Anxiety is often a huge part of PPD. Some say the anxiety came first; others feel their depression caused the anxiety, while others say it all feels like a jumbled mess of sadness and worry. Either way, anxiety is a common symptom of Postpartum Depression, which is one of several things that makes PPD different from a typical Major Depression. (Read Beyond Depression: Diagnosing Postpartum OCD)
6) Anger/irritability is common with Postpartum Depression. Frustration with all the changes that come with being a parent and/or having a newborn, anger about one’s symptoms, or irritability related to sleep loss/hormone shifts are definitely a “normal” part of PPD. (Read Understanding & Overcoming Anger: “I don’t want to be an angry person!”)
7) Guilt is a huge component of PPD. Guilt about having the illness, guilt about not being at your best when you wish you could be, guilt about your guilt. Guilt is one of the most common topics I address in therapy with postpartum women (and have had to address with myself, too). (Therapy can be a huge help in becoming free of all the guilt.)
8) The choice to breast or bottle-feed (or sometimes the lack of choice) often impacts PPD. Many women want to breastfeed, but struggle with it, and then feel terribly guilty switching to a bottle. Others realize, for their own health and wellness, they need to quit breastfeeding sooner than they’d wished. Too many are wrongly told they cannot breastfeed

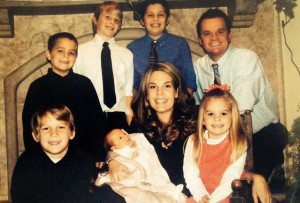
Singing & rocking my youngest, Sydney. Though I was able to breastfeed her, I introduced a bottle early on. I knew I needed it to help me survive PPD.
because they need a medication to help their depression or anxiety, and this leads to intense grief. Yes, breastfeeding (or not) is a hot topic when it comes to PPD.
9) Grief is usually a common part of Postpartum Depression. Most people don’t understand this or send the message that you should feel “happy” because of all you’ve gained in having a baby. And you surely have gained many blessings. But you’ve also lost many things: sleep, health, maybe breastfeeding or the ideal of what you thought would be, your figure, a sense of control, all these things listed above—the list goes on. Each loss must be grieved. (Read “How do I grieve?” Grief Work & TEARS)
10) PPD makes many women question their identity. “Who am I now?” is a common question. Many mothers feel lost, “not like myself,” or say, “I don’t know who I am anymore.” Rediscovering one’s identity after childbirth is common, and after PPD even more so.
11) Self-Esteem/sense of self is often deeply impacted by PPD. If you feel ashamed, guilty, angry, fearful, it can certainly lead to feelings of inadequacy as a mother and as a woman. All of these things can, and often do, make women question their self-worth. I’ve become an “expert” on self-worth because I’ve worked with so many women on this important topic (and personally, too.) Therapy is a great tool to help you learn to feel your true worth. (In the meantime, read this: How to Feel Self-Worth: The Pyramid of Self-Worth)
12) Relationship support can make or break you. Poor support or troubled relationships, especially with your husband/partner, are the number one non-biological cause of PPD. You need understanding, especially from those you love most, and when that doesn’t come, it can make postpartum depression/anxiety worse. On the flip side, PPD can be very hard on a relationship, so it’s important to seek help for both of you as needed. (Read more here: Couples & PPD)
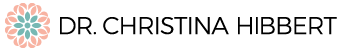
13) Women with PPD may seem “fine,” but often, it’s an act. Many people think, if a mom is depressed, she’ll obviously look like a mess, but that’s not the case. We want to feel fine. We try so hard to feel–and look–fine. But sometimes, though it seems we are, we’re not, not at all. (See my picture, below.)
14) Shame and embarrassment are a common part of postpartum depression and anxiety. Many women feel ashamed they aren’t “stronger” or more capable of simply “sucking it up” and “moving on.” Many feel embarrassed by their
Our family christmas photo, 2007, taken just three weeks after I gave birth and inherited my two nephews, going from 3 to 6 kids. My hardest postpartum experience by far, yet, don’t I look “fine?” Look closer. I definitely wasn’t. (Read about it in my memoir, “This is How We Grow.”)
symptoms. Unfortunately, the sting of the stigma of mental illness can feel especially sharp when you’ve just had a baby and so desperately want to be at your best.
15) For many PPD moms, it feels like no one gets it. Others might say they understand or even try to reach out and be supportive, but for many moms it feels like no one really gets PPD. Unless you’ve been there, it’s hard to truly relate, and unless you can truly relate, it’s hard for a PPD woman to want to open up and let you in. So, please, please, if you know a new mom, ask how she is feeling and really mean it. Listen to understand. Often we just need someone to sincerely ask so we can open up and begin healing.
16) Well-meaning friends/family often say/do the wrong things. When I had postpartum depression with my first son, who was colicky, one friend told me, “I really think babies reflect the temperament and calmness of their parents. That’s why I try to always be peaceful around my baby.” After my third baby was born, when I was officially a psychologist specializing in PPD and experiencing it again myself, a new friend asked, “Is that even real?” Statements like these can make PPD feel even worse and increase a mother’s sense of isolation.
17) Having Postpartum Depression in no way makes you a “slacker” or means you’re “lazy,” but many women feel that way. In fact, it’s often the high-achieving women with perfectionistic tendencies who fall prey to PPD. It’s one of the risk factors.
18) Because many PPD moms are used to being able to “do it all,” and do it all well, it can be hard for many of us to accept help. We know we need it, but when it comes down to it, it’s hard to let go of the need to do it on our own.
19) Help is out there, though it can be tough finding the right help. There are more PPD resources than ever. There is fabulous online support, solid educational programs, and providers who are compassionate and knowledgeable about pregnancy and postpartum mental health. The trouble often comes in accessing that help. My best advice? Stick with it. Help is out there, and it’s worth it to find the right kind of help for you. (PSI can help: www.postpartum.net)
20) Though we may fight it, medication is a good option for many pregnant and/or postpartum women. I wrote all about it here, so if you’re considering it, check this out. I also shared my own experience with choosing to take an antidepressant in my memoir, This is How We Grow: “I’ll admit, I do not want to take it. Must I?…I realize I haven’t really been living for far too long. I’ve been coping, surviving, manage, getting by—but coping is not living. I want to engage, set goals, dream, travel again…This little pill might just be the final ticket that helps me get there.” (p. 218) Sometimes, your brain just needs a little extra support, and medication is the one thing that might make the difference. (And yes, in many cases you can still breastfeed.) (More on medication: “Antidepressant? or Not? 12 Facts on Depression & Medication)
One final, bonus truth…
21) There is life after Postpartum Depression. With the right help, therapist and/or a support group specifically for PPD moms, you’ll find the understanding, information, and tools you need to be well again. Trust me when I say, six kids and eighteen years later, “There is life after PPD. With help, work, and time, you will be even better than better.”
If you’re a Postpartum Depression or Anxiety survivor, I’d love to hear from you. Do you agree with any of my “truths?” What are some truths of your own you’d like others to know? Let’s keep this important discussion going in the comments, below!
Be sure to check out Dr. Hibbert’s Award-Winning memoir, This is How We Grow!
Available now on Amazon.com.
FREE. Online. Growth. What more could you ask for?
You may manage your subscription options from your profile.
Let’s Connect…
“Like” my Facebook pages (Dr. Christina Hibbert; This Is How We Grow) and follow me on Twitter,Pinterest, & Instagram!
Related Articles/Posts:
Pregnancy & Postpartum Emotional Health
Postpartum Psychosis + Mental Health Stigma=40 Years in Prison? It’s time to speak up!
16 Things I’d Like My Postpartum Self to Know, 16 Years & 6 Kids Later (PSI Blog Hop)
PPD & Motherhood Mental Health: Self-Care & Letting Help In–The 2 Most Important Things
Postpartum Depression Treatment
Beyond Depression: Understanding Pregnancy/Postpartum OCD (Part 1)
Beyond Depression: Diagnosing Postpartum OCD (part 2) (& video)
Beyond Depression: Postpartum OCD Treatment (part 3) (& video)
Postpartum Depression Treatment: For Dads & Partners
Postpartum Depression Treatment: For Couples
Postpartum Depression Treatment: Complementary Alternative Modalities
Postpartum Depression Treatment: Psychotherapy
Postpartum Depression Treatment: Medication
Postpartum Depression Treatment: Self-Help
Postpartum Depression Treatment: Sleep
Postpartum Depression & Men: The Facts on Paternal Postnatal Depression
Mom Mental Health (& Happiness): The Importance of Alone Time
Mom Mental Health (part 2): How to Get Alone Time (25+ Strategies!)
Moving Beyond Shame: The Ultimate Power of Support & Time (PSI Blog Hop)
Pregnancy & Postpartum Mood & Anxiety Disorders: Are Women of Advanced Maternal Age at Higher Risk?
In Praise of Fathers: 10 Research-Based Ways Dads Impact Kids for the Better
5 Reasons Self-Esteem is a Myth
How to Feel Self-Worth: “The Pyramid of Self-Worth”
Thought Management, Part 1: The Relationship between Thoughts, Feelings, the Body, & Behavior
Womens’ Emotions & Hormones– Series
Achieving Balance–Why You’ve Got it Wrong, & How to Get it Right
Pregnancy & Postpartum Loss, Grief, & Family Healing (Part 1)
How to Cope with and Treat Perinatal Loss & Grief (Part 2)
Pregnancy/Postpartum Resources & Help:
Postpartum Support International Website
-Worldwide help and support for new mothers and families, including a bilingual hotline and state/country coordinators to help you find the right treatment provider or support in your area. PSI also provides educational courses on Perinatal Mood/Anxiety Disorders.
-Excellent source of education and support for mothers and families.
Arizona Postpartum Wellness Coalition
-Support for AZ families: Support Warmline, Brochures, & Provider/Family Education.
-Education & support for Providers and Families
Pregnancy & Postpartum Resources
**This article is not intended to replace proper medical/mental health care. If you think you may be suffering from Postpartum Depression or Anxiety, please contact your medical or mental health provider, or PSI, for referrals/help/support.**


So much yes. I struggled with ppd after the birth of my son and all these truths resonate with me. I it was the struggle of my life and it changed me, at the time in negative ways and now I am stronger than I have ever been. Transitioning to parenting in our modern digital world of commercialism and mixed messages has become the ultimate challenge that many women. face. Thank you a million times over for writing this. From the bottom of my heart.
You are so very welcome, Stephanie. So many of us struggle with PPD, and so many of us are forever changed by it. You’re so right–it can be the very thing that makes us stronger than we ever could have known. xoxo
Come check out my blog. I just put up a post about depression, antidepressants and creativity called “Making the most of my Monkey Mind”